How to Get a Project Started
The SVS Quality Improvement Committee has assembled the resources linked below to help any vascular team successfully start a new project for improving patient outcomes. If you have questions, please email svsquality@vascularsociety.org.
In addition, the SVS QIC has established a Quality Improvement (QI) Consulting Program, which is a free benefit to SVS members. The goal is to provide guidance to members performing quality improvement activities.
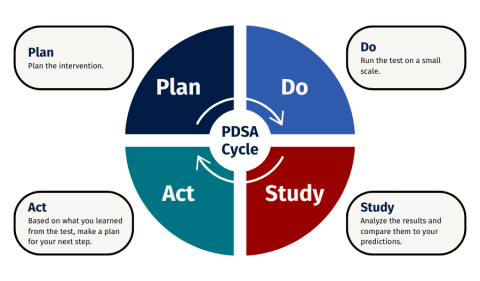
PDSA (Plan-Do-Study-Act) Framework for QI projects
What is the PDSA cycle?
While there are many different frameworks for organizing a project, the PDSA cycle is one of the most commonly utilized and referenced. PDSA stands for Plan-Do-Study-Act and this method originates from industry but is easily applied to the healthcare setting.
What are the steps of the PDSA cycle?
Plan
Start by asking: what are we trying to improve? Once you have identified an opportunity for improvement (see tips and tools), you then execute the following steps:
- Recruit a team
- Have a diverse team of members who have varying areas of expertise.
- Determine roles and responsibilities.
- Set timelines and a meeting schedule.
- Identify opportunities for improvement in the current process.
- Search the literature and interview experts to identify relevant best-evidence practices.
- Map out your existing process and compare the existing state to the desired state.
- Identify major steps in the process, who is involved and whether the steps are performed consistently.
- Identify if there are missing steps or areas where there is an opportunity to improve the steps. Also, take note of any wasted or areas of inefficiency if relevant.
- Tip: You may use a process map or swim lane map to organize the information and review with team members and other contributors. You can also utilize a pareto chart or fishbone diagrams in this step to brainstorm any specific causes of error or problems.
- Identify specific interventions that you feel will result in improvement in the process and outcome.
- Interventions should address the key drivers of error or problems identified in step two. A driver diagram can be used to organize this information.
- Tip: Focus on the low-hanging fruit. Considerations for interventions should prioritize simplicity rather than complexity such as improvements in existing processes instead of new processes. In addition, interventions that do not rely on memory are much more effective (ex. integration into an existing order set rather than providing education and reliance on memory
- When there are multiple possible interventions available, use your team to help prioritize a few changes as an initial start.
- Interventions should address the key drivers of error or problems identified in step two. A driver diagram can be used to organize this information.
- Draft a problem statement and a SMART goal: The problem statement helps clarify the specific problem. SMART stands for specific, measurable, achievable, relevant and time-bound and a SMART goal helps clarify what level of improvement you are hoping to achieve and in what time frame.
- Develop a project charter that includes the problem statement, SMART goal and also the process and outcome measure you will track and use to define success. The charter will also include the roles and responsibilities you outlined for your team earlier in the planning phase. See the template project charter here.
Do
Implement the proposed changes.
- It is vital to review the process changes with the process owners to anticipate any barriers, particularly if there are process owners who are not a part of your team.
- Have a plan for how to determine if the process changes are actually happening (ex. audits).
- It is helpful to have a specific kick-off date and a plan to celebrate early wins.
- Make sure involved team members have a clear way to report any unanticipated challenges or barriers.
- Have a plan for when and how to review the results with both your team and interested parties.
Study
- Gather data that is relevant to your SMART goal and review it regularly. The timeframe will vary depending on the process and how frequently it is utilized.
- Are there any unanticipated outcomes that have occurred as a result of your changes? These are often called balancing measures.
Act
- If your interventions have resulted in the desired outcome, then this step consists of making these changes permanent and identifying a plan for monitoring over time to address any new problems
- In many cases, there is some improvement but not at goal or perhaps no discernable change. If you can confirm that the proposed changes in the process are happening (ex. >80% compliance), then you should return to the PLAN phase and reevaluate. Multiple PDSA cycles may be utilized for a project.
Additional Information from the Institute for Healthcare Improvement (IHI)
- Whiteboard: The PDSA Cycle (Part 1) https://youtu.be/_-ceS9Ta820
- Whiteboard: The PDSA Cycle (Part 2) https://youtu.be/eYoJxjmv_QI
Supplemental Tips and Tools for Success
- How to decide where to start improving
- Data and Measurement in Quality Improvement
- Examples of measures (Donabedian)
- Repeat data tools with instructions (fishbone, driver, process map, run chart, pareto)
- How to get people on board