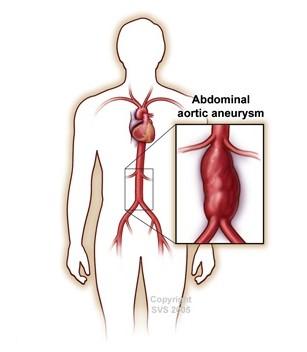
Patients with Abdominal Aortic Aneurysm (AAA)
Condition
Every year, 200,000 people in the U.S. are diagnosed with an abdominal aortic aneurysm (AAA), a dilation of the main artery within the abdomen.
A ruptured AAA is the 15th leading cause of death in the country (~4,500 cases/yr) and the 10th leading cause of death in men older than 55. AAAs occur in up to 13 percent of men and 6 percent of women over the age of 65.
Because the mortality associated with elective aneurysm repair is drastically lower than following repair of a ruptured AAA, the emphasis must be on early detection and repair prior to the occurrence of rupture.
Death from AAA is preventable with early detection and appropriate, timely treatment.
When to Refer
The Society for Vascular Surgery (SVS) has created disease-specific guidelines to assist in the care of patients at risk of with the diagnosis of AAA. Screening for AAA in specific patient populations has been shown to improve disease mortality and can be done without any patient risk using duplex ultrasound. The SVS recommends one-time screening for all patients >/= 65yo with any history of tobacco use as well as first degree relatives of AAA patients regardless of tobacco history. Any dilation of the aorta > 1.5 times its reference diameter is considered an aneurysm.
We recommend referral to a vascular surgeon at time of diagnosis of any AAA. Specific features that may prompt repair include: saccular morphology, size > 5cm in females, size > 5.5cm in males, or any symptoms such as back or abdominal pain or emboli to lower extremities that could be attributed to the AAA.
Why Refer to a Vascular Surgeon
Vascular surgery is the only discipline among the American Board of Medical Specialties which has specific training requirements to study the natural history, medical treatment, minimally invasive repair and traditional surgical repair options for your patients. A vascular surgeon can be your partner to help you and your patients get the most comprehensive management of their vascular disorder as well as the treatment that is best for them. Early referral and collaboration with a vascular surgeon can lead to better outcomes for each patient.
AAA: Useful Evidence-Based Guidelines for referring physicians
Screening of appropriate populations at increased risk and surveillance of identified AAAs is recommended; ultrasound is the preferred imaging tool.
| We recommend using ultrasound, when feasible, as the preferred imaging modality for aneurysm screening and surveillance. |
|---|
We recommend using ultrasound, when feasible, as the preferred imaging modality for aneurysm screening and surveillance.
| Level of Recommendation | 1 (Strong) |
| Quality of evidence | A (High) |
We suggest that the maximum aneurysm diameter derived from CT imaging should be based on an outer wall to outer wall measurement perpendicular to the path of the aorta.
| Level of recommendation | Good Practice Statement |
| Quality of evidence | Ungraded |
Who should be screened for AAA?
We recommend a one-time ultrasound screening for AAAs in men or women 65 to 75 years of age with a history of tobacco use.
| Level of Recommendation | 1 (Strong) |
| Quality of evidence | A (High) |
We suggest ultrasound screening for AAA in first-degree relatives of patients who present with an AAA. Screening should be performed in first-degree relatives who are between 65 and 75 years of age or in those older than 75 years and in good health.
| Level of recommendation | 2 (Weak) |
| Quality of evidence | C (Low) |
We suggest a one-time ultrasound screening for AAAs in men or women older than 75 years with a history of tobacco use and in otherwise good health who have not previously received a screening ultrasound.
| Level of recommendation | 2 (Weak) |
| Quality of evidence | (C (Low) |
If initial ultrasound screening identified an aortic diameter >2.5 cm but <3cm, we suggest rescreening after 10 years.
| Level of recommendation | 2 (Weak) |
| Quality of evidence | (C (Low) |
How often should surveillance be performed? Recommendations based on AAA diameter:
We suggest surveillance imaging at 3-year intervals for patients with an AAA between 3.0 and 3.9 cm.
| Level of recommendation | 2 (Weak) |
| Quality of evidence | (C (Low) |
We suggest surveillance imaging at 12-month intervals for patients with an AAA of 4.0 to 4.9 cm in diameter.
| Level of recommendation | 2 (Weak) |
| Quality of evidence | (C (Low) |
We suggest surveillance imaging at 6-month intervals for patients with an AAA between 5.0 and 5.4 cm in diameter.
| Level of recommendation | 2 (Weak) |
| Quality of evidence | (C (Low) |
We recommend CT imaging for patients thought to have symptomatic AAA (abdominal or back pain with known AAA, risk factors for AAA, etc.).
We recommend a CT scan to evaluate patients thought to have AAA presenting with recent-onset abdominal or back pain, particularly in the presence of a pulsatile epigastric mass or significant risk factors for AAA.
| Level of recommendation | 1 (Strong) |
| Quality of evidence | B (Moderate) |
Recommendations for referral and possible AAA repair:
- Referral to a vascular surgeon is recommended at the time of AAA diagnosis.
- Size criteria for repair
We suggest referral to a vascular surgeon at the time of initial diagnosis of an aortic aneurysm.
| Level of recommendation | Good Practice Statement |
| Quality of evidence | Ungraded |
We recommend repair for the patient who presents with an AAA and abdominal or back pain that is likely to be attributed to the aneurysm.
| Level of recommendation | 1 (Strong) |
| Quality of evidence | C (Low) |
We recommend elective repair for the patient at low or acceptable surgical risk with a fusiform AAA that is ≥5.5 cm.
| Level of recommendation | 1 (Strong) |
| Quality of evidence | A (High) |
We suggest elective repair for the patient who presents with a saccular aneurysm.
| Level of recommendation | 2 (Weak) |
| Quality of evidence | C (Low) |
We suggest repair in women with AAA between 5.0 cm and 5.4 cm in maximum diameter.
| Level of recommendation | 2 (Weak) |
Recommendations for smoking cessation and medical therapy in patients with AAA:
We recommend smoking cessation to reduce the risk of AAA growth and rupture.
| Level of recommendation | 1 (Strong) |
| Quality of evidence | B (Moderate) |
We suggest not administering statins, doxycycline, roxithromycin, ACE inhibitors, or angiotensin receptor blockers for the sole purpose of reducing the risk of AAA expansion and rupture.
| Level of recommendation | 2 (Weak) |
| Quality of evidence | (C (Low) |
We suggest not administering beta blocker therapy for the sole purpose of reducing the risk of AAA expansion and rupture.
| Level of recommendation | 1 (Strong) |
| Quality of evidence | B (Moderate) |
Further recommendations on Beta blocker therapy for patients with AAA:
We suggest continuation of beta blocker therapy during the perioperative period if it is part of an established medical regimen.
| Level of recommendation | 2 (Weak) |
| Quality of evidence | B (Moderate) |
If a decision was made to start beta blocker therapy (because of the presence of multiple risk factors, such as coronary artery disease, renal insufficiency, and diabetes), we suggest initiation well in advance of surgery to allow sufficient time to assess safety and tolerability.
| Level of recommendation | 2 (Weak) |
| Quality of evidence | B (Moderate) |
Recommendations for endovascular and open repair to optimize patient outcomes:
We suggest that elective EVAR be performed at centers with a volume of at least 10 EVAR cases each year and a documented perioperative mortality and conversion rate to OSR of 2% or less.
| Level of recommendation | 2 (Weak) |
| Quality of evidence | (C (Low) |
Shared decision-making with patients and referring providers:
1. Mortality risk
| Level of recommendation | 2 (Weak) |
| Quality of evidence | (C (Low) |
2. Concomitant major medical issues
| Quality of evidence | B (Moderate) |
In patients with a small aneurysm (4.0 cm to 5.4 cm) who will require chemotherapy, radiation therapy, or solid organ transplantation, we suggest a shared decision-making approach to decide about treatment options.
| Level of recommendation | 2 (Weak) |
| Quality of evidence | (C (Low) |
Recommendations for follow-up after Open surgical AAA repair and EVAR: Longitudinal care is important for all vascular patients, especially so after EVAR (Endovascular Aneurysm repair)
After EVAR:
We recommend baseline imaging in the first month after EVAR with contrast-enhanced CT and color duplex ultrasound imaging. In the absence of an endoleak or sac enlargement, imaging should be repeated in 12 months using contrast-enhanced CT or color duplex ultrasound imaging.
| Level of recommendation | 1 (Strong) |
| Quality of evidence | B (Moderate) |
If a type II endoleak is observed 1 month after EVAR, we suggest postoperative surveillance with contrast-enhanced CT and color duplex ultrasound imaging at 6 months.
If neither endoleak nor AAA enlargement is observed 1 year after EVAR, we suggest color duplex ultrasound when feasible, or CT imaging if ultrasound is not possible, for annual surveillance.
| Level of recommendation | 2 (Weak) |
| Quality of evidence | (C (Low) |
If a type II endoleak is associated with an aneurysm sac that is shrinking or stable in size, we suggest color duplex ultrasound for continued surveillance at 6-month intervals for 24 months and then annually thereafter.
| Level of recommendation | 2 (Weak) |
| Quality of evidence | (C (Low) |
If a new endoleak is detected, we suggest evaluation for a type I or type III endoleak.
| Level of recommendation | 2 (Weak) |
| Quality of evidence | (C (Low) |
We suggest noncontrast-enhanced CT imaging of the entire aorta at 5-year intervals after open repair or EVAR.
| Level of recommendation | 2 (Weak) |
| Quality of evidence | (C (Low) |
After Open Repair:
We recommend that follow-up of patients after aneurysm repair include a thorough lower extremity pulse examination or ABI.
| Level of recommendation | 1 (Strong) |
| Quality of evidence | B (Moderate) |
We recommend a prompt evaluation for possible graft limb occlusion if patients develop new-onset lower extremity claudication, ischemia, or reduction in ABI after aneurysm repair.
| Level of recommendation | 1 (Strong) |
| Quality of evidence | A (High) |
Source:
The Society for Vascular Surgery practice guidelines on the care of patients with an abdominal aortic aneurysm
Elliot L. Chaikof, MD, PhD, Ronald L. Dalman, MD, Mark K. Eskandari, MD, Benjamin M. Jackson, MD, W. Anthony Lee, MD, M. Ashraf Mansour, MD, Tara M. Mastracci, MD, Matthew Mell, MD, M. Hassan Murad, MD, MPH, Louis L. Nguyen, MD, MBA, MPH, Gustavo S. Oderich, MD, Madhukar S. Patel, MD, MBA, ScM, Marc L. Schermerhorn, MD, MPH, Benjamin W. Starnes, MD
J Vasc Surg 2018; 67(1):2-77.
https://doi.org/10.1016/j.jvs.2017.10.044