SVS & SVSF Celebrate Hispanic Heritage Month
The SVS and SVS Foundation join together to celebrate Hispanic Heritage Month, celebrated from Sept. 15-Oct. 15. The SVS and SVSF have created the Voices of Vascular Series to aid in the expansion of diversity, equity and inclusion initiatives throughout each entity. Visit this webpage throughout the months of September and October to explore profiles of various SVS members with Hispanic heritage.
Funding the Future of Vascular Health
Your gift to the SVS Foundation is an investment into vascular health – past, present and future - while also supporting the mission of the SVSF! Learn more and make your gift today!
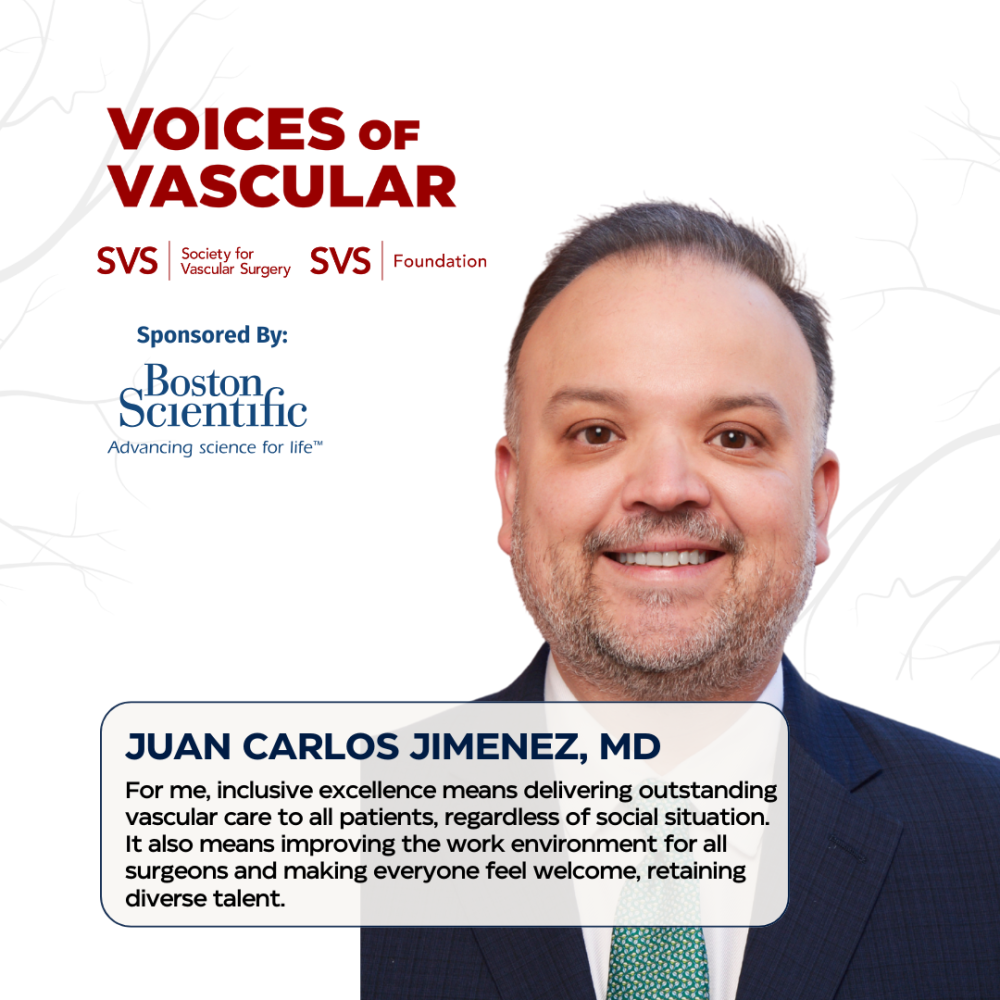
HHM Member Feature
Dr. Juan Carlos Jimenez, a vascular surgeon and assistant dean for faculty initiatives at the University of California, Los Angeles (UCLA) medical school, carries a legacy of service shaped by his family’s immigrant journey and his father’s dedication to community care.
Concepción Montaño Ramírez, RN
Concepción Montaño Ramírez, RN, a familiar name to many who participate in the SVS Foundation September Vascular Health Step Challenge, has been the challenge’s Top Walker for the past three years.
Jesús G. Ulloa, MD
Born in 1983 to migrant farm workers in Yuba City, California, Dr. Jesús G. Ulloa’s roots are firmly planted in the values of hard work and family. He and his wife, an ophthalmologist, and his two young children reside in Southern California, ensuring a close connection with other family members.
Daphne Nunille González Muñoz, MD
Dr. Daphne Nunille González Muñoz’s story is one of perseverance, passion and purpose, an example of how one person's dedication can ripple across borders and generations.
Luis Sanchez, MD
Dr. Luis Sanchez’s story is a testament to the power of mentorship, innovation and representation in vascular medicine. Born and raised in Puerto Rico, Dr. Sanchez spent his formative years attending high school on the island and pursued his academic career in the Northeast, earning his undergraduate degree at Yale University, followed by medical school at Harvard Medical School.
Past Voices of Vascular Profiles
Hispanic Heritage Month Health Facts
Throughout Hispanic Heritage Month, visit this page to view facts regarding vascular health for the Hispanic/ Latinx population.
Cuban Americans have the highest rates of peripheral arterial disease in diverse Hispanic/Latino communities:
Compared with Mexican Americans, Cuban Americans have a threefold higher odds for the presence of peripheral arterial disease (PAD) independent of educational attainment, immigrant generation, and traditional cardiovascular disease (CVD) risk factors.
2022 Heart Disease & Stroke Statistical Update Fact Sheet Hispanic/Latino Race & Cardiovascular Diseases*:
Among U.S. Hispanic adults 20 years of age and older from 2015 to 2018, 52.3% of males and 42.7% of females had cardiovascular disease (CVD).
Hispanics and African Americans Receive Lower Extremity Endovascular Interventions in the Late Stages of Peripheral Artery Disease With Higher Risks of Amputation:
Racial minorities received the endovascular surgical care in the late stages of the peripheral artery disease and overall had higher risks of undergoing an amputation in postoperative 30 days as compared with the non-hispanic whites (NHW) population.
Cardiovascular Disease in Hispanics/Latinos in the United States:
Data from the National Alliance for Hispanic Health (NHIS) showed that in 2012, only 15.7% of Hispanics adults age ≥18 years met the national guidelines for physical activity and Hispanic adults (39.8%) were more likely to be physically inactive that NHW adults (26.2%).
Reporting and representation of ethnic minorities in cardiovascular trials: A systematic review
22% of Hispanic and Latinx men and women are likely to develop PAD.
Yale researchers call for strategies to eliminate inequities in access to peripheral artery disease care among adults who share a Hispanic background:
Using a national database, a Yale research team identified 1,018,220 PAD hospitalizations. Between 2011-2017, they discovered that compared with non-Hispanic patients, Hispanics adults with severe PAD had longer hospitalizations. These patients were more often admitted through the emergency department and received less revascularization procedures and underwent more amputations.
Thank you to our Companion Sponsor!
The SVS and SVS Foundation extend their sincerest gratitude to Boston ScientificTM for being the Companion Sponsor for our celebration of Hispanic Heritage Month.

