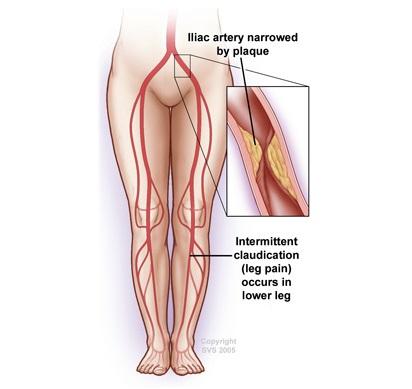
Aortoiliac occlusive disease is the narrowing or blockage of the aorta, the main blood vessel in your body, or the iliac arteries. The iliac arteries are the branches that your aorta divides into around the level of the belly button to provide blood to your legs and the organs in your pelvis. This blockage is typically caused by a buildup of plaque within the walls of your blood vessels.
The aorta and iliac arteries are the second most common blood vessels to be affected by peripheral arterial disease (PAD) after the blood vessels in the thigh. PAD occurs in 12-20% of people over the age of 65.
- The most common cause of aortoiliac disease is atherosclerosis (hardening of the arteries). Hardening of the arteries may be caused by smoking, high cholesterol, high blood pressure, diabetes, genetic predisposition or obesity.
- Inflammatory conditions such as Takayasu’s arteritis may cause inflammation in the arteries causing blockages of the arteries.
- Radiation to the pelvis may cause progressive inflammation in the arterial wall leading to blockages of the arteries.

May Be Absent
You may have varied symptoms or no symptoms at all and still have aortoiliac occlusive disease.
Fatigue, Pain, or Cramping When Walking
When felt in the buttocks, thighs or calves, these symptoms may signal mild to moderate aortoiliac occlusive disease. As the disease progresses, these symptoms may occur after walking very short distances.
Erectile Dysfunction
Men may experience erectile dysfunction.
Pain at Rest, Leg and Feet Problems
In severe cases, you may feel pain in your feet or toes at rest, coldness and numbness in your legs, sores or wounds on your legs and feet, and even gangrene or the death of tissue in your feet.
See a Vascular Surgeon
You will be asked questions about symptoms and medical history, including questions about family members. The vascular surgeon will also perform a physical exam.
Tests May Be Recommended
Initially an ankle-brachial index test and a duplex ultrasound may be recommended.
If further testing is needed a CT angiogram, MR angiogram, or a catheter-directed angiogram are options. These studies use different types of dye to help identify where blockages in the arteries are located to plan further treatment. With a CT angiogram and MR angiogram, dye is delivered through an IV. With a catheter-directed angiogram, dye is injected through a thin tube (catheter) inserted in an artery.

Aortoiliac occlusive disease may be managed by:
- Risk factor modification, such as quitting smoking, controlling cholesterol or high blood pressure, managing diabetes and regular exercise.
- Medication may be prescribed, such as an aspirin or another medication to prevent platelets from clotting in the blood. A statin drug helps to control cholesterol and help prevent plaque progression.
If further treatment is needed, a minimally invasive procedure or a surgical bypass may be considered.
- The most common minimally invasive treatment is the placement of a stent in your aorta or iliac arteries. This procedure is commonly done at the same time as a catheter-directed angiogram. The stent is a small device that opens the blockage in the arteries to create a wider path for blood flow to the lower half of your body. An angioplasty, in which an inflatable balloon device is inserted through the catheter to further assist in opening up the arteries, can be added to the treatment.
- A surgical bypass is the creation of a detour around the blockage. The detour may start in the aorta and may end either in the iliac arteries in your pelvis, or in an artery in your groin or leg. A bypass may be performed either on one or both sides at the same time, usually using an artificial graft. If there is not a suitable artery to originate the bypass in the aorta, or if you are not healthy enough to undergo an aortic-based procedure, the bypass generally starts at the axillary artery underneath the collarbone and ends in one or both legs.
- The best way to prevent development of aortoiliac occlusive disease is to not smoke, and manage cholesterol, blood pressure and diabetes.
- If you do smoke, ask your vascular surgeon to help you find a smoking cessation program that will work for you.
- Get regular exercise.
- Eat a healthy, well-balanced diet that is low in fat and cholesterol.
