What is CVI?
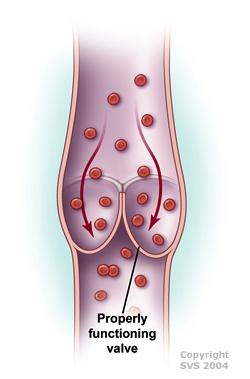
If you have Chronic Venous Insufficiency (CVI), the valves in your veins (usually in the leg or sometimes the arms) don't work, causing blood to pool in your legs and putting increased pressure on the walls of the veins. It can be due to valve dysfunction (usually hereditary) or even valve destruction after a deep vein thrombosis (DVT) or blood clot.
CVI is a fairly common and usually chronic condition that may affect up to 40% of the U.S population. It's more common in women (especially after multiple pregnancies) and in people who are middle-aged or older.
CVI is treatable, and preventing complications is important to maintaining your overall health.
Most symptoms are mild, and not limb-threatening. This can include:
- Swelling in the legs or ankles
- Tight feeling or heaviness in the calves
- Itchy or painful legs
- Pain or discomfort while walking that improves with rest (claudication)
- Brown-colored skin, typically around the ankles
- Visible varicose veins
- Hard-to-treat leg ulcers
- Restless legs syndrome, causing an uncomfortable urge to move the legs
- Painful leg cramps or muscle spasms
- Damage to vein valves due to aging or injury
- Obesity
- Pregnancy
- Family history of venous disease
- Prolonged standing or sitting
- Deep vein thrombosis (blood clots)
- Smoking
- Lack of physical activity
Talk to a Doctor
If you are experiencing any symptoms of CVI, you should talk to your doctor about a referral to see a Vascular Surgeon.
Early detection and management can help prevent complications and improve the quality of life for those with CVI.
Role of a Vascular Surgeon
A comprehensive evaluation by a vascular surgeon is necessary for an accurate diagnosis and to develop an appropriate treatment plan for CVI.
Diagnosis
For diagnosis, your doctor typically conducts a thorough medical history and physical examination to assess symptoms and risk factors. You might also be referred for a duplex ultrasound, which evaluates blood flow and vein structure. Other imaging tests may be used to further assess vein health and function.
Your specific treatment plan depends on the severity of the condition and individual factors. Most treatment is nonsurgical. The main goal is to prevent severe swelling and ulcers from developing.
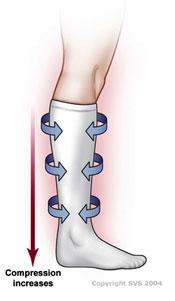
- Lifestyle modifications, such as elevating the legs, regular exercise, and wearing compression stockings to improve blood flow
- Medications to reduce inflammation and manage symptoms
- Minimally invasive procedures, such as endovenous ablation or sclerotherapy to close off damaged veins
- Surgical interventions, such as vein ligation or stripping for severe cases
- Supportive measures, which include wound care for ulcers and management of associated complications