What are Varicose Veins?
Varicose veins are swollen, blue, bulging, twisted veins that appear under the skin on your legs.
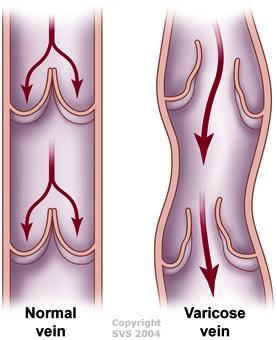
They are caused by high pressure inside the leg veins from valves that are damaged and not working properly, as gravity puts constant pressure on them while they work to return blood from your feet to your heart. Genetics can play a big role in whether or not you develop them.
As many as 40 million Americans have varicose veins. If left untreated, varicose veins can get worse. They can cause leg aches, fatigue and skin changes like rashes, redness, leg swelling, blood clots, or sores.
Treatment can help improve your quality of life plus leg and general circulatory health.
Below, the left picture shows a healthy vein with working valves that stop blood from flowing backward. The right picture shows a weak vein with valves that don't work properly, letting blood flow the wrong way toward the feet. This increases pressure in the vein causing the varicose veins.
Did you know? Venous valves are one-way valves in our veins that help blood move up from our feet and legs to the heart. They stop the blood from flowing back down to the feet due to gravity.
- Visible veins that are swollen, twisted, or bulging
- Thin, web-like veins close to the skin's surface
- Aching or heaviness in the legs, especially after prolonged standing or sitting
- Swelling, particularly around the ankles
- Itching or burning sensation around the veins
- Discomfort or pain that worsens with prolonged standing or sitting
- Skin changes, such as redness, inflammation, or sores
- Restless legs or leg cramps, especially at night
- Age: People between the ages of 30 and 70
- Pregnancy: 50-55% of American women experience varicose veins during pregnancy. Most of the time, the veins return to normal within a year after childbirth.
- Multiple pregnancies: Women who have multiple pregnancies may develop permanent varicose veins.
- Family history
- Obesity
- Standing or sitting for long periods of time
Diagnosis and Role of Vascular Surgeon
A vascular surgeon will ask you about your symptoms and medical history. They will also do a physical exam that includes gently probing for problem areas on your legs while you are standing.
Your vascular surgeon might also perform a duplex ultrasound test, which uses high-frequency sound waves to measure the blood flow in your veins. This helps pinpoint problem veins and determine the best way to treat them.
There are several treatment options that can help varicose veins.
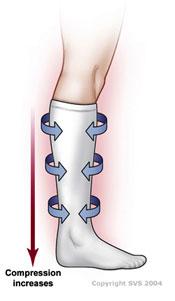
Compression Stockings
Knee-high compression stockings, usually that provide 20-30 mmHg of compression, will often help relieve symptoms such as aching or swelling. These stockings compress the veins and prevent blood from traveling down pooling in the legs. If you have insurance, most companies require that you wear compression stockings for at least three months before covering any other type of treatment for varicose veins.
Lifestyle Changes
Most doctors will suggest additional lifestyle changes such as:
- Starting a walking program
- Maintaining a healthy weight
- Elevating legs when resting
- Avoiding sitting or standing for long periods of time
Additional Treatments
In some cases, a vascular surgeon will recommend additional treatments for varicose veins:
Ablation Therapy
If compression stockings don't provide sufficient relief, some form of ablation therapy (laser, radiofrequency, or adhesive injection) of a superficial vein (the great and/or small saphenous vein) may be an option for you.
Treatment is administered at the vascular surgeon's office. Your leg will be cleansed, and sterile drapes placed. Your vascular surgeon will then inject numbing medication and insert a catheter (thin tube) into the vein. Typically, patients feel only the injection of numbing medicine. The tube is advanced through the entire vein and then all the surrounding skin is numbed if necessary. The ablation catheter then treats the vein by closing it off so it can no longer reflux or “back leak” into the varicose veins. After the procedure, the leg is placed in a compression stocking or wrapped with a compression bandage.
Microphlebectomy
Microphlebectomy is a minimally invasive, surgical technique used to treat varicose veins that are near the surface of the skin and too large for sclerotherapy. This procedure is also known as "ambulatory phlebectomy" or "stab avulsion."
Patients are usually given local anesthesia along the course of the vein to be removed. The skin over the vein is cleaned and marked for incisions. Your vascular surgeon will make very small incisions (2-3 mm) are made over the varicose vein. Using specialized hooks or instruments, the vein is gently pulled out through the small incisions in segments.
The incisions are typically so small that they don’t require stitches and heal naturally, often leaving minimal scarring. Patients usually wear compression stockings to support healing and reduce swelling. You can usually return to normal activities within a day or two, with complete recovery almost immediately.
Sclerotherapy
Sclerotherapy may be recommended if the affected veins are twisted and not straight enough. With the help of ultrasound, a small needle is used to inject sclerosant, a chemical that causes the vein to spasm and clot. This type of clot is not dangerous. It is broken down by your body's natural processes making your varicose vein disappear. Small "spider" veins can be treated this way using an even smaller needle.
Vein Stripping
Vein stripping is a procedure used to treat severe varicose veins. Your vascular surgeon makes two small incisions, one in the groin area and one below the knee, to remove the diseased veins. This is an outpatient procedure, usually done under general anesthesia. Most patients can usually return to their normal activities after four weeks.
Post Treatment
After treatment, you should continue to wear compression stockings to help prevent new varicose veins from forming and to speed recovery time.