What is DVT?
Deep vein thrombosis (DVT) happens when a blood clot (thrombus) forms in a deep vein, usually in the legs. This clot can partially or completely block blood flow through the vein.
If a piece of the clot breaks off, it could travel to one of your lungs and make it hard to breathe or even cause death.
DVT is considered a medical emergency and requires prompt diagnosis and treatment to prevent complications. Treatment can last from weeks to months.
Nearly 300,000 first-time cases of DVT occur in the U.S. every year.
- DVT can occur without any warning signs
- Swelling in the affected leg, often in the calf or thigh
- Pain or tenderness, which may worsen when standing or walking
- Warmth and redness over the affected area of the leg
- Skin discoloration, such as a bluish or reddish hue
- Swollen veins that are visible or palpable
- Leg fatigue or heaviness
- In severe cases, DVT may lead to symptoms of pulmonary embolism, such as sudden shortness of breath, chest pain, rapid heartbeat, or coughing up blood.
You should seek medical attention right away if you experience any DVT symptoms.
- Inactivity: Such as after long flights or bed rest after surgery.
- Surgery: Certain surgeries, especially those involving the legs or abdomen.
- Trauma: Injury to the veins, such as fractures or severe muscle injury.
- Obesity: Obesity can increase pressure on the veins and impair blood flow.
- Pregnancy: Pregnancy and childbirth due to hormonal changes, increased pressure on the veins, and decreased mobility.
- Medications: Certain medications, such as birth control pills or hormone replacement therapy.
- Smoking: Smoking since it damages blood vessels.
- Family history: A family history of blood clotting disorders or a personal history of previous DVT increases the risk of developing the condition.
- Older Age: Particularly people 60 and older.
- Medical conditions: Certain medical conditions, such as cancer, heart disease, inflammatory bowel disease, and inherited blood clotting disorders.
Talk to a Doctor
You should talk to a doctor if you experience any DVT symptoms, such as swelling, pain, warmth, or redness in one leg. In addition, if you have risk factors, it's important to share that with your doctor.
Prompt medical evaluation is crucial to diagnose DVT early and prevent complications.
Role of Vascular Surgeon
Vascular surgeons play a key role in diagnosing DVT, which typically involves a combination of clinical evaluation, imaging tests, and laboratory studies.
Diagnosis
To diagnosis DVT, your doctor will ask you about your symptoms, medical history, and risk factors. They will also perform a physical examination, looking for swelling, tenderness, redness, or warmth in the affected limb.
They might recommend tests such as:
- D-dimer blood test: A D-dimer test measures the levels of a substance called D-dimer in the blood. D-dimer is released when a blood clot dissolves. Elevated D-dimer levels may indicate the presence of a blood clot, although this test alone is not sufficient to diagnose DVT and is often used in conjunction with imaging tests.
- Imaging tests: Diagnostic imaging tests often are used to determine if a blood clot is present and identify its location and extent. The most commonly used imaging tests include:
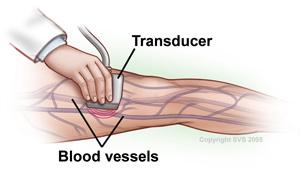
- Doppler ultrasound: This non-invasive test uses sound waves to create images of blood flow in the veins. It can detect blood clots and evaluate blood flow characteristics.
- Venography: In this procedure, a contrast dye is injected into a vein, and X-ray images are taken to visualize the veins and identify any blockages caused by blood clots.
- Computed Tomography Angiography (CTA) and Magnetic Resonance Angiography (MRA) Tests: These tests can create detailed images of the veins and detect blood clots.
Once DVT is diagnosed, you many need further evaluation to determine the underlying cause and assess your risk of complications. DVT is usually treated with medication.
Blood Thinners
Blood thinners are also known as anticoagulants. These are the most common medicines used for treating DVT. They prevent blood clots from getting larger by decreasing your blood's ability to clot. Over time, your body works with the blood thinners to decrease the size and consistency of the clot. Blood thinners can be taken as a pill, as an injection or through an IV. Blood thinners can increase your chance of bleeding, so careful follow-up with your vascular surgeon is essential.
Percutaneous Thrombectomy
Percutaneous Thrombectomy is a minimally invasive procedure that removes blood clots from veins. This is typically used in new DVT cases. Your vascular surgeon will use specialized devices, inserted through a small puncture, into a vein to remove the blood clot.
If they find an underlying narrowing, then an angioplasty may be performed to expand your vein. Sometimes a stent is needed for larger veins, such as the iliac veins or inferior vena cava.
Thrombolytic Therapy
Thrombolytic Therapy is sometimes used to quickly dissolve a blood clot, especially if the clot is large and causing severe symptoms. This treatment brings a much higher risk of bleeding than blood thinners, so it is not used unless truly necessary.
An IVC Filter
In rare cases, where anticoagulant therapy is contraindicated or ineffective, or if there is a high risk of pulmonary embolism, an inferior vena cava (IVC) filter may be placed into the inferior vena cava, one of the largest veins in the body. The filter does not stop a blood clot from forming, but can prevent a large clot from entering your lungs.
