What is CAD?
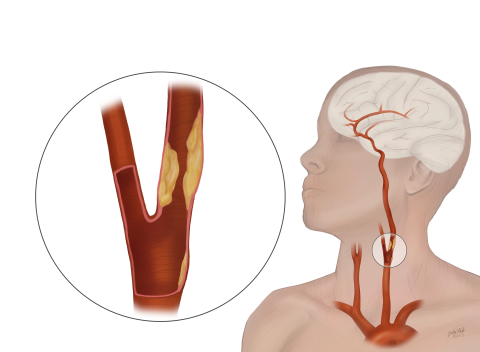
The carotid arteries are the main arteries in your neck that supply blood to your brain.
As you age, the carotid arteries build up “plaque,” which is a sticky substance made of fat and cholesterol. Plaque narrows your arteries and makes them stiff. This process is called atherosclerosis or "hardening of the arteries.”
Carotid artery disease (CAD) occurs when the carotid arteries become narrowed or blocked due to plaque buildup. This narrowing, also called carotid artery stenosis, can lead to strokes or “mini-strokes.”
Up to 3% of individuals older than 65 have CAD. Your risk increases as you age and if you have a history of smoking, high blood pressure, high cholesterol, diabetes or heart disease. CAD is responsible for up to one-third of all strokes.
About 700,000 strokes occur every year. Stroke causes 1 in every 15 deaths.
You might not have any symptoms in the early stages of CAD. Sometimes, the first sign of the disease is a stroke.
However, strokes typically have warning signs — mini-strokes, also called transient ischemic attacks (TIAs). TIA symptoms are usually temporary, lasting a few minutes to a few hours. TIAs should be treated as serious medical emergencies, and they require immediate medical attention.
Some symptoms of TIA and stroke include:
- Weakness, numbness, or tingling on one side of the body
- Inability to control movement of a body part
- Loss of vision or blurred vision in one or both eyes
- Inability to speak clearly
- Difficulty talking or comprehending what others are saying
Talk to a Doctor
If you think you are having a stroke or TIA, you should get emergency medical help right away.
Diagnosis
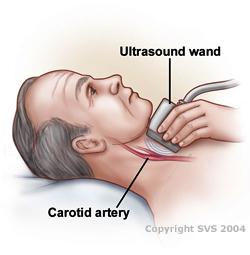
If your doctor thinks you might have CAD, they will recommend a noninvasive carotid duplex ultrasound exam. The ultrasound results will confirm if you have CAD and its severity.
Role of a Vascular Surgeon
If CAD is confirmed or suspected, you may be referred to a vascular surgeon. Vascular surgeons are experts in the diagnosis, medical management, and all of the procedural options (surgery, stents) to treat CAD.
It's important to treat CAD to lower your risk of stroke or prevent another stroke. Treatment depends on how severe your condition is and may include:
- Medication: Often a combination of medications can help slow the progression of CAD and reduce the risk of stroke. Aspirin and other medications (like clopidogrel, prasugrel, ticagrelor) that “thin” the blood decrease your risk of stroke. Medications that lower your cholesterol and blood pressure are also commonly prescribed to keep the blockage from getting worse. Your doctor may adjust your medication over time.
- Quitting Smoking: This is important for managing CAD and for your overall health.
- Surgery: If the degree of narrowing is more than 60%, in addition to medication, you may need surgery.
- Carotid artery stenting: A less invasive procedure in which a stent (small mesh tube) is placed in the artery to keep it open.
Some people with CAD benefit from surgery even if they don’t have symptoms.
