Thrombolytic therapy is the administration of drugs called lytics or “clot busters” to dissolve blood clots that have acutely (suddenly) blocked your major arteries or veins and pose potentially serious or life-threatening implications. To be effective, the therapy needs to be initiated as soon as possible, before permanent damage has occurred.
The length of a treatment session varies depending on the underlying cause. A session can take from 60 minutes (typical for a heart attack) to 48 hours (often the case for deep vein thrombosis, or DVT).
This therapy can reverse or reduce the adverse effects of:
- Blocked arteries of the brain (stroke).
- Blocked arteries of the heart (heart attack).
- Blocked arteries of the lung (pulmonary embolism).
- Blocked veins of the leg (deep vein thrombosis/DVT).
- Blocked arteries of the leg (acute arterial thrombosis /leg ischemia).
- Blocked surgical bypasses, blocked dialysis fistulas or catheters.
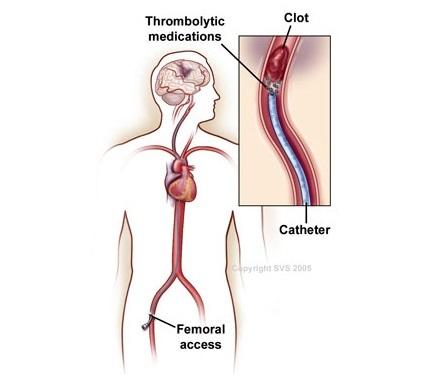
There are two ways clot-busting agents (lytics) can be given: through a peripheral IV (systemic thrombolysis) or through a catheter (thin tube) that has been navigated to the site of the clot.
Systemic thrombolysis is used for heart attack, stroke and pulmonary embolism.
- The “clot-busting” drug will be delivered through a peripheral intravenous (IV) line, usually through a visible vein in your arm.
- Performed at your bedside in an intensive care unit while your heart and lung functions are monitored.
- The drug circulates within the blood stream until it reaches the clot. This may lessen the drug’s effect because of dilution, or higher doses may be needed increasing the chance of bleeding.
The main risk of this therapy is bleeding. Approximately 5% of treated patients will have a major bleed, while the risk of bleeding in the brain (stroke) is roughly 1%. If either occurs during treatment, it will stop immediately.
Bleeding can occur from any puncture sites on the skin used to insert IVs, or any other fresh wound or injury site.
Spontaneous bleeding can also develop, including:
- Blood in the urine.
- Nosebleed.
- Bloody stools.
- Unexpected or unusually heavy vaginal bleeding.
- Brain bleed (stroke).
Another possible risk is embolization. As the clot softens and dissolves, small pieces may break off and travel deeper in the affected organ (e.g., leg or lungs), worsening the symptoms.
- Thrombolysis is usually an emergency treatment. If you are diagnosed with a condition that can be treated with thrombolysis you will be transferred to an intensive care unit for close monitoring of your heart and lung functions.
- You may be asked to fast, particularly if you will have catheter-directed thrombolysis.
Most of the time, treatment will reverse or alleviate your symptoms. However, thrombolytic therapy is not always successful and may not dissolve the blood clot, particularly if initiation of treatment was delayed. Other times, even if the clot has dissolved the affected tissues (your heart, brain, lungs or leg) may be permanently damaged due to prolonged restriction of blood flow.
- After treatment, your vascular surgeon will re-assess your symptoms. Imaging tests (e.g., CT scan, echocardiogram, arteriogram or venogram) may be needed to check for any residual blood clot.
- Depending on the underlying cause of clot formation your vascular surgeon may suggest further treatment—some kind of minimally invasive procedure (e.g. balloon angioplasty, stenting or open surgery).
- You will eventually be placed on blood thinners (anticoagulants), which may include heparin and warfarin (Coumadin).
- Even with successful treatment, the clot may redevelop in the same blood vessel. If so, more aggressive treatment will be needed to address the underlying causes of the blood clot and repair damaged tissues and organs.
