What is PAD?
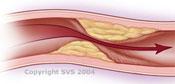
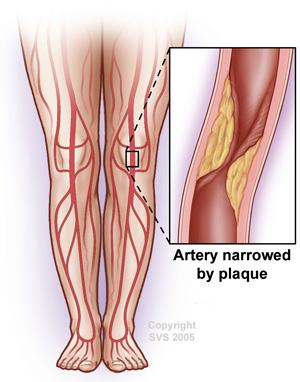
Peripheral Artery Disease (PAD) is a chronic condition where plaque builds up in the arteries that carry blood to your legs. “Plaque” is a sticky substance made of fat and cholesterol. Over time, this plaque can gradually narrow the arteries. If it progresses, blood flow in that artery can become partially or completely blocked.
When this happens, blood can’t freely provide oxygen, glucose and other essential nutrients to your legs. This can cause pain, cramps, or discomfort in your legs, especially when you walk or exercise. Left untreated, PAD can lead to serious complications, including amputation and death.
PAD affects more than 10 million people in the U.S. It is more common in people 65 years and older but can occur at nearly any age. Smoking, diabetes, high blood pressure, high cholesterol or triglycerides, obesity, and kidney disease increase your risk for PAD.
- No Symptoms: Many people with PAD may not notice any symptoms, especially in the early stages. It’s important to know the risk factors for PAD and talk to your doctor about your possible risk.
- Pain or Cramping While Walking (Claudication): Claudication is pain, cramping, or discomfort in the muscles in your legs (calves, thighs, or buttocks) or arms, that happens during physical activity like walking or exercising. The pain stops when you rest and returns when you start the activity again.
- Pain in Toes or Feet While Resting: When PAD worsens, you might also have pain in your feet when resting (especially at night).
- Sores on Toes or Feet that Won’t Heal: An open wound or ulcer on your toes or feet, often at a pressure point on the foot. An ulcer can progress to gangrene. These symptoms require prompt medical attention.
- Leg Numbness or Weakness: You may experience numbness or weakness in the legs, making it harder to walk or stand for longer periods of time.
- Coldness in Your Lower Leg or Foot: One leg or foot may feel colder to the touch than the other due to restricted blood flow.
- Change in Skin Color: The skin on your legs may turn pale, bluish, or have a shiny appearance.
- Slow Nail or Hair Growth on Your Legs: Poor circulation can slow down nail and hair growth on your legs and feet, which can lead to little or no hair on the toes, feet, or lower legs.
Talk to a Doctor
Leg pain does not always mean you have PAD. However, if you are older or have other risk factors, you should ask your doctor if you should be assessed for PAD.
You should seek an urgent referral to a vascular surgeon if you experience pain when resting — especially at night — or foot sores that won’t heal.
Diagnosis
To diagnose PAD and determine its severity, your doctor may recommend:
- A non-invasive test called the ankle brachial index (ABI). This test checks your blood pressure at your ankle and compares it to the blood pressure in your arm.
- An arterial Doppler which uses ultrasound to evaluate the blood vessels for plaque, flow, and blockage.
- An X-ray called an angiogram. This procedure finds out where the plaque has built up in your arteries. It can be done with a CT scan, an MRI, or by puncturing an artery in your groin or wrist and injecting contrast dye.
Role of Vascular Surgeon
If you experience symptoms or have been diagnosed with PAD, ask your primary care provider to refer you to a vascular surgeon. Vascular surgeons can confirm your diagnosis and perform necessary treatments, including medication management, exercise therapy, minimally invasive “endovascular” procedures, and open surgery.
Treatment for PAD is important in the early and mid-stages to prevent the disease from progressing and to avoid procedures that might otherwise become necessary. In advanced stages, treatment is critical to avoid amputation.
If you have PAD, treatment can include:
- Daily exercise, like walking
- Quitting smoking
- Medication
If PAD is causing serious symptoms, treatment might also include:
- Atherectomy
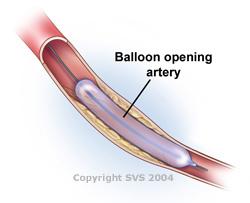
- Balloon angioplasty
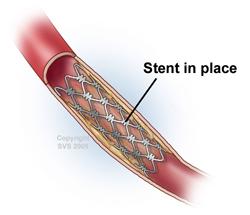
- Stent placement
- Surgical bypass
These procedures can be very effective in improving the blood flow of your affected leg.