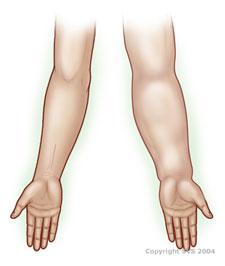
Lymphedema is an accumulation of lymph fluid in the soft tissues, most frequently in the arms or legs. Lymph fluid, rich in protein, is normally filtered by the lymph nodes and is then released into the bloodstream. When the nodes are obstructed, their filtering capacity is overwhelmed and lymph fluid collects and causes swelling.
Usually chronic, but can be controlled
Lymphedema is usually a chronic condition. Untreated, lymphedema can lead to irreversible skin changes, frequent infections, reduced mobility of the affected limb and diminished quality of life.
- Swelling, Heaviness, Tightness & Itching: You may notice swelling and heaviness in the affected limb or other body part, along with tightness and itching.
- Progressive Swelling: You may experience progressive swelling that causes significantly reduced mobility of the affected limb.
- Skin Problems: Infections, Hardening & Thickening: In advanced stages, lymphedema can cause recurrent skin infections, irreversible soft tissue swelling, and, finally, hardening and thickening of the skin.
Primary Lymphedema is due to failed or faulty development of lymph nodes and/or blood vessels and mainly affects women. This deficiency may be present at birth, but symptoms often appear later in life. Primary lymphedema most often occurs in the legs but can affect the entire body.
Secondary Lymphedema is typically caused by surgical removal, injury or destruction of the lymph nodes or of blood vessels as a complication of radiation treatment, or by a tropical parasitic infection called lymphatic filariasis (elephantiasis). It can also develop from a chronic overload of the lymphatic system due to recurrent skin infections, problems with blood vessels or obesity. Secondary lymphedema is most often localized to the body part with the absent or injured lymph nodes.
A history of painless leg swelling experienced as a teenager or at any age following removal or damage to lymph nodes may suggest lymphedema. A diagnosis can often be confirmed by a physical exam of the affected limb or body part.
Tests May Be Needed
Imaging of the lymphatic system through lymphoscintigraphy is sometimes performed to identify treatment options.
Early, aggressive treatment is the key to achieving long-term control of lymphedema.
At Stage I, when there is “no permanent soft tissue changes,” swelling can be reversed by elevating the affected limb and by wearing compression garments.
At Stage II, lymphedema requires treatment for relief of symptoms as some scarring has occurred in the affected tissues.
In Stage III, when definite skin thickening and hardening have occurred, treatment consists of reduction and maintenance therapy.
- Reduction Therapy involves compression wrapping with low-stretch bandages worn 24 hours a day, supplemented with massage therapy and exercise.
- Maintenance Therapy involves regular daytime use of compression garments and/or pneumatic compression sleeves that inflate and deflate to help propel lymphatic fluid.
In intractable cases, surgery to remove excess tissue or bypass obstructed lymph vessels may be considered, but results are mixed.

Here are ways to manage lymphedema:
- Wear compression garments and use prescribed pumps for the rest of your life.
- Elevate the affected limb.
- Exercise regularly at a moderate level while wearing compression garments.
- Eat a nutritious, balanced, low salt diet.
- Take good care of the skin on your affected limb or body part.
- Wear protective clothing to protect your skin from injury.
- Cleanse your skin and keep it well moisturized.
- Guard against infections and fungi.
